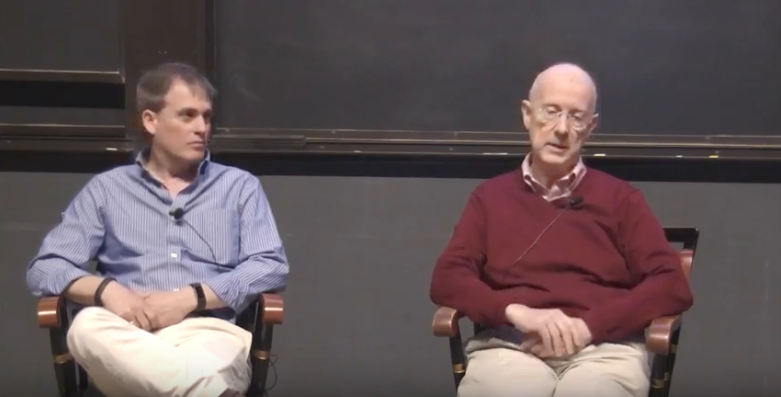
The Affordable Care Act faces an uncertain future. With the Republicans again seeking to push through a potential new health law, Joseph Newhouse and Michael Chernew spoke at an HMS Talk at 12 to discuss the state of health care today and the potential directions the Republicans (and future leaders) might take.
Chernew and Newhouse wouldn’t speculate on what a new bill would look like, but they did analyze several aspects of the current health care space:
The ACA has had a measurable difference in coverage expansion, but some of its gains could deteriorate
According to Newhouse, Obamacare has helped to fill gaps in Medicare drug coverage, enabled Medicaid expansion (but, since it’s optional for states, 19 have not taken up the provision), and created the insurance exchanges.
It’s the last portion that’s suffering the most currently. If the cost-sharing subsidies that help insurers are not continued, they could deteriorate rapidly. Trump has waffled on the cost subsidy issue since taking office, but insurers will need greater clarity on where the issue stands as they submit bids in the coming weeks.
The Republicans have the power to negatively impact the ACA even if they can’t agree on legislation. “Don’t think that just because a bill doesn’t pass, the ACA will be able to function in the same way that it has,” says Chernew.
Other current ways to curtail spending haven’t been perfected
Because health spending is inevitably financed by the population at large in some way, the key issues are how much money is spent and how the burden of that spending is distributed. Many individuals must pay more than their share of the cost to finance care for the highest risk beneficiaries. Taxes or higher premiums for this lower risk group are the primary ways to achieve this end.
According to Chernew, policymakers could also charge the high risk patients more, or have them pay more at the point of service. The current administration, thus far, appears to favor these less generous health plans that impose less collective risk pooling, in which case the sicker pay more for care.
However, no financing scheme will survive if the rate of health care spending growth is not slowed. The ACA has somewhat lowered spending, but “we haven’t really cracked that nut yet,” says Chernew.
There is bipartisan support for new payment models that shift accountability for spending towards service providers, who then would have the incentive to coordinate care and find efficiencies. Evidence suggests only modest savings. For the foreseeable future, the alternative seems to be slower increases in fees. There’s a long way to go to prove these new models can be successful on a large scale.
“We’re still at the beginning of that process,” says Chernew.
The talk was also covered by Harvard Medical School news.
Enjoy content like this? Sign up for our newsletter and follow HCP on Twitter.