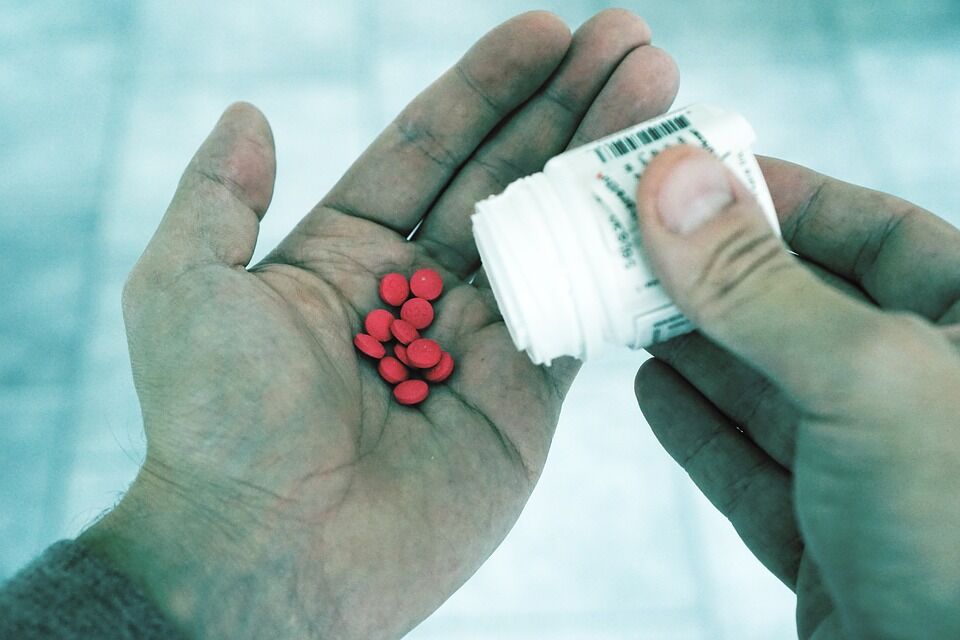
The United States has found itself in the middle of an opioid epidemic spurred by the overuse of prescription opioids. Patients are put at risk for long-term opioid use, misuse, overdose, and death by long-duration and high-dose initial prescriptions.
However, a call for more restraint in physician prescribing has led to a decline in monthly opioid prescriptions among patients that have not used opioids before, and a decrease of providers initiating opioid therapy. Department of Health Care Policy Seidman Fellow Wenjia Zhu, PhD, Leonard D. Schaffer Professor of Health Care Policy Michael E. Chernew, PhD, associate physician policy researcher at the RAND Corporation Tisamarie B. Sherry, MD, PhD, and associate professor of health care policy Nicole Maestas, MPP, PhD, highlight this decline in a study in the New England Journal of Medicine, but warn that there is still more room for improvement.
As the epidemic progresses, many providers have stopped initiating opioid therapy. From July 2012 to December 2017, the monthly prescribing rate of opioid prescriptions among patients who had not previously used opioids (called “opioid naïve”) decreased by 54%. These first-time prescriptions have become a main target in reducing the risk of opioid abuse as they are seen as a gateway to long-term use.
While many physicians have discontinued the initiation of opioid therapy, there is a subset of clinicians that have continued prescribing opioids to opioid naïve patients. Some of these physicians are practicing risky prescribing: prescribing a morphine-equivalent dose of 50 milligrams per day or more, or any dose prescribed for longer than three days. A portion of these prescriptions are for over 90 morphine- equivalent milligrams per day, which places patients at risk of both nonfatal and fatal overdoses.
Although the decrease in initial opioid prescription appears positive, there is a drawback. Large numbers of providers have stopped initiating opioid therapy altogether, raising the possibility that in some instances patients could be experiencing under-treated pain, especially if preferred methods of pain relief have failed.
“The ultimate goal is to promote safer prescribing that balances the importance of pain relief with the risks of opioid treatment, rather than an all-or-nothing approach,” Maestas told the Harvard Gazette. “There can be appropriate indications and circumstances for using opioids, although the list of medical indications for which opioids are considered appropriate is getting smaller and smaller.”
The study urges further analysis to understand the circumstances in which high-risk opioids are prescribed as a way to inform opioid control policies that aim to strike a balance between preserving access to pain control when necessary while reducing inappropriate use.
This study has been featured in Time , The American Journal of Managed Care, U.S. News & World Report, Reuters,Psychiatric & Behavioral Health Learning Network, Gizmodo, M.D. Alert, KFGO, Cision , Digital Journal, and Pain News Network.